The seminal vesicle is an essential accessory gland in the male reproductive system, contributing significantly to the formation of semen by secreting seminal fluid. One of the critical aspects of its function is the lining epithelium, which plays a pivotal role in producing and regulating the secretion of seminal components. The lining epithelium of the seminal vesicle is specialized to facilitate the secretion of fructose, prostaglandins, and other proteins that nourish and support sperm viability. Studying the histology and function of this epithelium provides insight into reproductive health, fertility, and the overall physiology of the male reproductive system.
Structure of the Seminal Vesicle
The seminal vesicle is a paired gland located posterior to the bladder and lateral to the vas deferens. Its structure is highly convoluted, consisting of coiled tubular glands lined with specialized epithelium. The gland wall is composed of three main layers the mucosa, muscularis, and adventitia. The mucosa, where the lining epithelium resides, is highly folded to maximize surface area for secretion. The epithelium interacts closely with underlying connective tissue and smooth muscle to regulate seminal fluid production and release during ejaculation.
Lining Epithelium Characteristics
The lining epithelium of the seminal vesicle is typically a pseudostratified columnar epithelium with secretory cells. This means that while the epithelium appears to have multiple layers, all cells are in contact with the basement membrane, allowing coordinated secretory activity. The secretory cells are tall, column-shaped, and contain abundant cytoplasm rich in secretory vesicles and glycogen granules. These cells are responsible for producing the viscous, fructose-rich fluid that provides energy for sperm motility.
Secretory Functions of the Epithelium
The seminal vesicle epithelium plays a critical role in male fertility through the secretion of seminal plasma components. Fructose is a primary energy source for sperm, supporting motility and survival after ejaculation. Prostaglandins secreted by the epithelium contribute to the modulation of female reproductive tract contractions, aiding sperm transport toward the ovum. Additionally, the epithelium secretes various proteins, enzymes, and mucins that enhance sperm function, protect sperm from oxidative damage, and facilitate the formation of a coagulum to temporarily trap sperm, ensuring effective delivery.
Cellular Organization
The epithelium contains several specialized cell types
- Secretory Columnar CellsThese are the predominant cell type, producing seminal fluid components such as fructose and prostaglandins.
- Basal CellsLocated near the basement membrane, these cells act as progenitor cells, ensuring epithelial renewal and maintenance.
- Interspersed Secretory CellsSome cells exhibit vesicle-rich cytoplasm, releasing proteins and enzymes into the lumen through exocytosis.
Histological Features
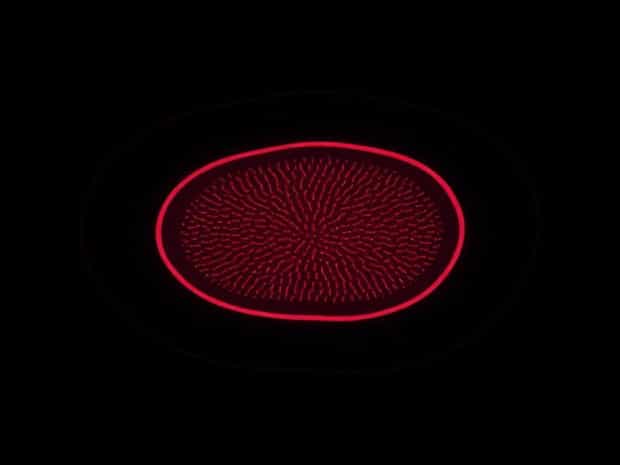
Under the microscope, the seminal vesicle epithelium appears highly folded and lined by columnar cells with large, oval nuclei positioned basally. The cytoplasm often contains secretory granules that stain variably depending on the histological technique. The pseudostratified arrangement allows maximal secretory efficiency while maintaining structural integrity. Microvilli on the apical surface of epithelial cells increase the absorptive and secretory surface area, enhancing the production of seminal fluid components. The epithelium is supported by a thin layer of connective tissue containing blood vessels, nerves, and lymphatics, which supply nutrients and remove waste products.
Functional Adaptations
The lining epithelium is adapted to the gland’s function in several ways
- Its tall, columnar cells provide a large cytoplasmic volume for active secretion.
- Pseudostratification allows high cell density and continuous epithelial renewal.
- Secretory granules and vesicles enable rapid release of seminal fluid during ejaculation.
- Microvilli and mucosal folds maximize surface area for secretion and absorption.
Regulation of Epithelial Secretion
The secretory activity of the seminal vesicle epithelium is regulated by hormonal and neural signals. Androgens, particularly testosterone, are critical for maintaining epithelial structure and stimulating secretion. The epithelial cells respond to androgenic stimulation by producing fructose, prostaglandins, and other seminal components. Neural signals, including parasympathetic stimulation, trigger contraction of the muscularis layer, facilitating the expulsion of seminal fluid into the ejaculatory duct. Dysregulation of these signals can lead to reduced seminal volume, decreased sperm motility, and impaired fertility.
Clinical Significance
Understanding the lining epithelium of the seminal vesicle has important clinical implications. Conditions such as seminal vesiculitis, obstruction, or epithelial atrophy can reduce the quality and quantity of seminal fluid, directly impacting male fertility. Histological examination of the epithelium can help diagnose infections, inflammatory disorders, or structural abnormalities. Additionally, age-related changes in the epithelial lining may lead to decreased secretory function, highlighting the importance of epithelial health in reproductive outcomes.
Comparative Aspects
The seminal vesicle epithelium varies across species. In humans, it is highly pseudostratified and columnar, whereas in rodents, the epithelium may display more pronounced secretory granules and less prominent folds. Comparative studies indicate that the secretory capacity and cellular organization of the epithelium are closely linked to reproductive strategies and the volume of seminal fluid required for successful fertilization. Such differences underline the evolutionary adaptations of the lining epithelium to species-specific reproductive demands.
Research and Future Directions
Ongoing research into the seminal vesicle epithelium focuses on understanding molecular pathways regulating secretion, epithelial regeneration, and responses to hormonal changes. Advances in imaging, molecular biology, and tissue engineering may allow scientists to develop new treatments for male infertility linked to epithelial dysfunction. Additionally, studies on epithelial secretory mechanisms can provide insights into male reproductive physiology and potential contraceptive strategies targeting seminal fluid production.
The lining epithelium of the seminal vesicle is a highly specialized structure essential for the production of seminal fluid components that support sperm viability and reproductive success. Its pseudostratified columnar arrangement, secretory granules, microvilli, and hormonal responsiveness enable efficient secretion of fructose, prostaglandins, and proteins necessary for sperm motility and fertilization. By maintaining structural integrity and functional adaptability, the epithelial lining ensures the seminal vesicle fulfills its role in male reproductive physiology. Understanding its histology, regulation, and clinical significance is crucial for insights into fertility, reproductive health, and the evolutionary adaptations of male accessory glands.