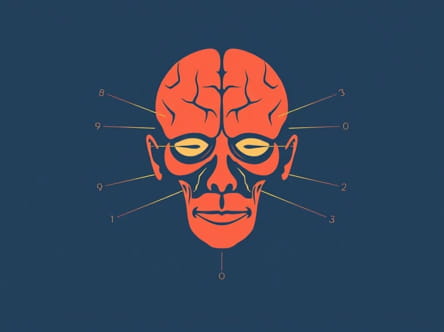
The gag reflex is a vital protective mechanism of the human body, preventing foreign objects from entering the throat and airway. It is an involuntary response that involves multiple cranial nerves, primarily cranial nerve IX (glossopharyngeal nerve) and cranial nerve X (vagus nerve). This reflex is not only essential for swallowing and airway protection but also serves as an important neurological indicator in clinical examinations. Understanding the anatomy, physiology, and clinical significance of the gag reflex is crucial for medical professionals and anyone interested in human neurology.
Anatomy and Physiology of the Gag Reflex
The gag reflex is a complex neuromuscular response that involves the coordinated action of sensory and motor pathways. It is primarily mediated by cranial nerves IX and X, which serve distinct but interconnected roles in detecting stimuli and triggering muscular responses.
Cranial Nerve IX Glossopharyngeal Nerve
The glossopharyngeal nerve is responsible for the sensory component of the gag reflex. When the posterior part of the tongue, soft palate, or pharyngeal wall is stimulated, sensory signals are transmitted via cranial nerve IX to the medulla oblongata, where the reflex arc is processed.
- FunctionDetects touch, taste, and pain in the posterior third of the tongue and pharynx.
- Reflex RoleInitiates the sensory signal that prompts the motor response for gagging.
- Clinical SignificanceDamage to cranial nerve IX may result in diminished or absent gag reflex, which can indicate neurological impairment.
Cranial Nerve X Vagus Nerve
The vagus nerve provides the motor response for the gag reflex. Once the sensory signal is processed, cranial nerve X activates the muscles of the pharynx and soft palate, causing a contraction that prevents foreign objects from entering the throat.
- FunctionControls muscles involved in swallowing, speech, and airway protection.
- Reflex RoleTriggers the pharyngeal contraction that constitutes the gag reflex.
- Clinical SignificanceDysfunction of cranial nerve X can lead to impaired swallowing, voice changes, and aspiration risk.
Mechanism of the Gag Reflex
The gag reflex is initiated when a stimulus, such as touch or pressure, is applied to the posterior pharyngeal wall or back of the tongue. The glossopharyngeal nerve senses the stimulus and sends the information to the medullary centers of the brainstem. The vagus nerve then coordinates the motor response, causing contraction of the pharyngeal muscles and elevation of the soft palate. This action effectively closes off the airway, preventing foreign objects from reaching the lungs.
Steps of Reflex Arc
- Stimulation of the posterior pharynx or tongue.
- Transmission of sensory signals via cranial nerve IX to the medulla oblongata.
- Processing of the signal in the brainstem centers.
- Activation of cranial nerve X to induce motor response.
- Contraction of pharyngeal and palatal muscles, resulting in gagging.
Clinical Significance of the Gag Reflex
The gag reflex is not only a protective mechanism but also an essential neurological indicator. Clinicians often assess the presence, absence, or exaggeration of the gag reflex to evaluate cranial nerve function and detect potential neurological disorders.
Neurological Examination
During a neurological assessment, testing the gag reflex can help identify lesions or damage to cranial nerves IX and X. An absent or weakened reflex may suggest issues such as stroke, brainstem injury, or peripheral nerve damage. Conversely, an exaggerated gag reflex can indicate hyperreflexia associated with certain neurological conditions.
Implications for Swallowing and Airway Protection
A properly functioning gag reflex is crucial for safe swallowing and preventing aspiration. Impairment of this reflex increases the risk of choking and respiratory complications. In patients with neurological diseases, such as amyotrophic lateral sclerosis or multiple sclerosis, careful monitoring of the gag reflex is essential to prevent aspiration pneumonia and other complications.
Considerations in Medical Procedures
Understanding the gag reflex is also important in dentistry, endoscopy, and other medical procedures involving the oral cavity or throat. Excessive gagging can complicate procedures, while an absent reflex may indicate a need for precautions to protect the airway. Techniques such as desensitization, topical anesthetics, and patient positioning are often used to manage gag reflex during procedures.
Factors Affecting the Gag Reflex
The sensitivity of the gag reflex varies among individuals and can be influenced by age, anxiety, prior medical conditions, and even habitual suppression. Some people may have an extremely sensitive gag reflex, making medical and dental procedures challenging, while others may have a diminished reflex due to neurological impairment or habituation.
Age-Related Changes
With aging, the gag reflex may become less sensitive, which can increase the risk of aspiration. This change is particularly important for elderly patients during swallowing assessments or when managing feeding and oral hygiene.
Anxiety and Psychological Factors
Anxiety and anticipation of gagging can enhance reflex sensitivity. Behavioral techniques, relaxation exercises, and desensitization can help reduce the exaggerated gag reflex during medical procedures.
The gag reflex is a critical protective mechanism mediated by cranial nerves IX and X. The glossopharyngeal nerve provides sensory input, while the vagus nerve executes the motor response that safeguards the airway. Clinically, the gag reflex is a valuable tool for assessing neurological function, ensuring safe swallowing, and guiding medical procedures. Understanding its anatomy, physiology, and factors affecting its sensitivity allows healthcare professionals to manage patients safely, prevent complications, and optimize care in both routine and emergency settings. The integration of knowledge about cranial nerves IX and X and the gag reflex remains fundamental for neurologists, dentists, speech therapists, and other healthcare providers.