In the field of neuro-ophthalmology, understanding the difference between congruous and incongruous visual field defects is crucial for diagnosing various brain and eye conditions. Visual field testing is often performed when patients experience partial loss of sight or unusual blind spots, as these patterns can reveal the exact location of the damage within the visual pathways. Although both terms describe abnormalities in the visual field, the degree of similarity between the affected areas in each eye is what sets them apart. This distinction is not just theoretical it plays a vital role in pinpointing the underlying cause, whether it is a lesion in the optic tract, lateral geniculate body, or occipital cortex. By recognizing the visual field patterns and correlating them with brain anatomy, eye specialists can provide more accurate diagnoses and treatment plans.
Understanding Visual Field Defects
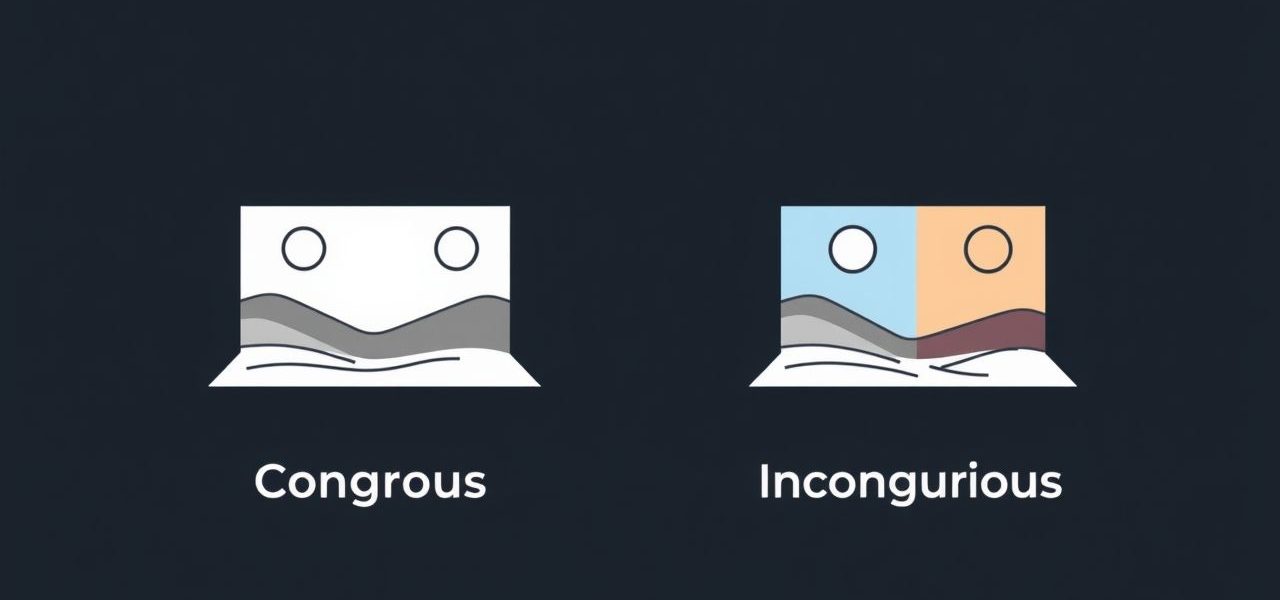
The visual field refers to the entire area a person can see when the eyes are fixed in one position. Damage to different parts of the visual pathway from the retina to the occipital cortex can cause specific patterns of vision loss. These patterns are often classified as congruous or incongruous based on their appearance in each eye. The classification depends on how closely the affected areas in both eyes match in shape and location.
Definition of Congruous Visual Field Defects
Congruous visual field defects occur when the vision loss pattern in both eyes is nearly identical in size, shape, and location. This high degree of similarity suggests that the lesion causing the problem is located further back in the visual pathway, closer to the occipital lobe. Because the nerve fibers are more precisely organized in the posterior parts of the brain, damage in these areas tends to produce perfectly or nearly perfectly matched defects.
Common Causes of Congruous Visual Field Defects
- Occipital lobe lesions, often due to stroke or trauma
- Posterior cerebral artery infarctions
- Brain tumors affecting the occipital cortex
- Inflammatory or demyelinating diseases like multiple sclerosis
Patients with these defects often have predictable blind spots that make it easier for specialists to locate the exact site of the lesion through imaging studies and visual field mapping.
Definition of Incongruous Visual Field Defects
Incongruous visual field defects, on the other hand, occur when the vision loss patterns in each eye are similar in general location but differ in size, shape, or extent. This type of defect usually points to a lesion located earlier in the visual pathway, such as in the optic tract or lateral geniculate body, where the nerve fibers are less precisely aligned compared to the occipital cortex.
Common Causes of Incongruous Visual Field Defects
- Optic tract lesions from tumors or vascular events
- Damage to the lateral geniculate body
- Early compression by mass lesions in the temporal or parietal lobe
- Traumatic brain injury affecting the anterior visual pathways
In these cases, the variation in the field loss between the eyes can help localize the lesion more anteriorly compared to congruous defects.
Key Differences Between Congruous and Incongruous Defects
Although both types of defects indicate problems within the visual pathways, their differences are important for diagnosis
- Location of LesionCongruous defects suggest posterior lesions (occipital lobe), while incongruous defects suggest more anterior lesions (optic tract, lateral geniculate body).
- Pattern SimilarityCongruous defects are almost identical in both eyes, while incongruous defects show variation.
- Diagnostic ValueCongruity helps clinicians narrow down the site of damage within the visual pathway.
Role of Visual Pathway Anatomy
The arrangement of nerve fibers within the visual pathway explains why congruity increases as you move further back in the brain. In the anterior pathways, fibers from each eye are mixed but not yet perfectly aligned. As these fibers reach the occipital cortex, they become highly organized, which is why lesions there produce defects with a high degree of similarity between eyes.
Clinical Examples
Case of a Congruous Visual Field Defect
A patient experiences sudden right-sided vision loss in both eyes. Visual field testing shows a nearly identical right homonymous hemianopia. MRI confirms a left occipital lobe stroke. The high degree of congruity pointed to a posterior lesion even before imaging was done.
Case of an Incongruous Visual Field Defect
Another patient presents with blurred vision and patchy loss on the left side of their visual field. Testing reveals a left homonymous hemianopia, but with the pattern slightly larger in one eye. MRI shows a lesion in the right optic tract due to a compressive tumor. The incongruity suggested a more anterior lesion site.
Diagnostic Importance in Eye and Brain Disorders
Recognizing whether a defect is congruous or incongruous is an essential skill for eye specialists and neurologists. This evaluation can
- Guide imaging toward the correct part of the brain
- Differentiate between cortical and subcortical lesions
- Assist in early detection of tumors, strokes, or demyelinating diseases
- Help plan appropriate treatment and rehabilitation
Testing for Congruity
The gold standard for detecting and classifying these defects is automated perimetry, which maps a patient’s visual field with high precision. In addition to automated tests, confrontation visual field testing can provide quick bedside screening, though it is less detailed. Interpreting these results alongside patient symptoms and neuroimaging is essential for accurate diagnosis.
Management and Follow-Up
While congruity itself does not determine treatment, identifying the type of visual field defect helps find the cause, which in turn dictates management. For example
- Stroke-related occipital lobe lesions may require anticoagulation or blood pressure control
- Tumor-related optic tract compression may need surgical removal
- Demyelinating lesions may respond to corticosteroid therapy
Follow-up testing is essential to monitor changes in the visual field and assess whether interventions are working.
Understanding the difference between congruous and incongruous visual field defects is more than just an academic distinction it is a valuable diagnostic tool in neuro-ophthalmology. By recognizing the degree of similarity in vision loss between the eyes, clinicians can localize lesions within the visual pathway and guide further testing and treatment. This knowledge not only improves diagnostic accuracy but also enhances patient outcomes by ensuring that the underlying condition is addressed promptly and appropriately.