Pustular psoriasis flare ups can be overwhelming, painful, and emotionally distressing for those who experience them. Unlike milder forms of psoriasis that cause red, scaly patches on the skin, pustular psoriasis is more severe and is characterized by white or yellow pus-filled blisters surrounded by inflamed skin. These flare ups may come suddenly, spread rapidly, and require immediate medical attention. Understanding what triggers these episodes, how they affect the body, and what treatment options exist can help patients better manage their symptoms and reduce the frequency of flare ups.
What is Pustular Psoriasis?
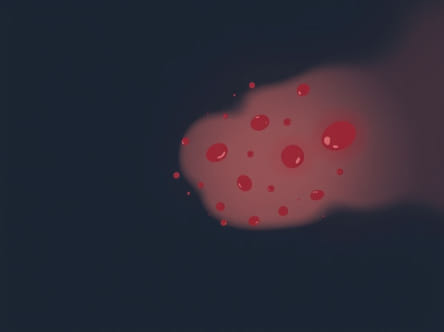
Pustular psoriasis is a rare and serious type of psoriasis that can affect small areas of the skin or cover large portions of the body. It is not an infection, even though the pustules contain pus. Instead, the blisters are filled with white blood cells and occur due to an immune system malfunction. During a flare up, the skin becomes red, tender, and covered with pus-filled bumps that may dry and peel after a few days.
This condition may occur in localized forms, such as palmoplantar pustulosis (on the hands and feet), or in a more generalized form that spreads widely across the body. Flare ups are often accompanied by systemic symptoms, making them more than just a skin condition.
Symptoms of a Pustular Psoriasis Flare Up
Flare ups vary in intensity but typically involve sudden outbreaks of pustules that may appear within hours. Symptoms may include
- Red, inflamed skin covered with white or yellow pustules
- Severe itching or burning sensation
- Dry, cracked skin after pustules dry out
- Swelling and tenderness in affected areas
- Fever, chills, and fatigue during widespread flare ups
- Dehydration and rapid heart rate in severe cases
Because flare ups can affect the whole body, they may also lead to serious complications if left untreated. For this reason, medical intervention is often necessary.
Causes and Triggers of Flare Ups
Pustular psoriasis flare ups are caused by abnormal immune system activity, but several factors can trigger an outbreak. Common triggers include
- Sudden withdrawal of corticosteroid medications– Stopping steroids abruptly can cause flare ups.
- Stress– Emotional or physical stress often worsens symptoms.
- Infections– Bacterial or viral illnesses can trigger immune system responses.
- Skin injury– Cuts, burns, or irritation may cause new pustules.
- Medications– Certain drugs such as lithium, beta-blockers, or antimalarials may provoke outbreaks.
- Hormonal changes– Fluctuations, especially in women, may contribute to flare ups.
- Environmental factors– Cold weather, smoking, or chemical exposure can aggravate the condition.
Identifying and avoiding triggers is one of the most important steps in reducing the frequency of pustular psoriasis flare ups.
Types of Pustular Psoriasis Flare Ups
Generalized Pustular Psoriasis
This severe form affects large portions of the body and often appears suddenly. It may cause fever, chills, nausea, rapid pulse, and dehydration. Generalized flare ups require urgent medical attention because they can become life-threatening.
Palmoplantar Pustulosis
This localized type affects the palms of the hands and soles of the feet. Flare ups can make walking or using the hands very painful. While not life-threatening, this form can greatly affect quality of life.
Acrodermatitis Continua of Hallopeau
A rare type that affects fingertips or toes. Flare ups may cause pustules near the nails and lead to nail loss if untreated.
Diagnosis During a Flare Up
To diagnose pustular psoriasis flare ups, doctors usually perform a physical examination of the skin, review medical history, and may order additional tests such as
- Skin biopsy to rule out infections
- Blood tests to check for inflammation or infection markers
- Imaging tests in cases where joints are involved
Because pustular psoriasis can resemble other skin conditions, accurate diagnosis is essential for proper treatment.
Treatment Options for Flare Ups
Managing a pustular psoriasis flare up usually requires a combination of medical treatment, lifestyle adjustments, and supportive care. Treatment may include
Topical Treatments
For mild or localized flare ups, doctors may prescribe creams and ointments such as corticosteroids, coal tar preparations, or vitamin D analogues to reduce inflammation and scaling.
Systemic Medications
Severe or generalized flare ups often require systemic medications, including
- Methotrexate – Reduces immune system activity
- Cyclosporine – Suppresses immune response
- Acitretin – A retinoid that helps normalize skin cell growth
- Biologics – Target specific immune system proteins involved in psoriasis
These medications are usually reserved for more severe flare ups due to their potential side effects.
Light Therapy
Some patients benefit from phototherapy, which involves controlled exposure to ultraviolet light. This treatment can slow down the rapid skin cell turnover seen in pustular psoriasis.
Supportive Care
During severe flare ups, hospitalization may be necessary to provide IV fluids, antibiotics if secondary infections occur, and close monitoring of vital signs.
Lifestyle and Home Remedies
While medical treatment is essential, lifestyle changes can also help manage pustular psoriasis flare ups. Patients may benefit from
- Keeping skin moisturized with fragrance-free creams
- Taking warm baths with soothing additives like oatmeal
- Wearing soft, breathable clothing to reduce irritation
- Managing stress through relaxation techniques or counseling
- Avoiding smoking and alcohol, which can trigger flare ups
- Following a healthy diet rich in anti-inflammatory foods
These supportive measures can make flare ups less severe and reduce overall discomfort.
Complications of Pustular Psoriasis Flare Ups
If not treated properly, flare ups can lead to serious complications. These may include
- Secondary skin infections
- Liver or kidney strain due to systemic inflammation
- Joint involvement leading to psoriatic arthritis
- Emotional distress and depression due to visible skin changes
Because pustular psoriasis flare ups can affect both physical and mental health, early treatment and ongoing support are critical.
Prevention of Flare Ups
Although pustular psoriasis cannot be completely prevented, patients can reduce the risk of flare ups by
- Avoiding sudden withdrawal of prescribed medications
- Managing stress with regular exercise, meditation, or yoga
- Protecting skin from injury and irritation
- Following medical advice and adhering to treatment plans
- Scheduling regular check-ups with a dermatologist
Preventive care plays an important role in minimizing the severity and frequency of pustular psoriasis flare ups.
Pustular psoriasis flare ups are a serious health concern that require timely medical attention and long-term management. By recognizing symptoms early, understanding triggers, and following a comprehensive treatment plan, patients can reduce the intensity of flare ups and improve their quality of life. With ongoing research and advances in treatment, more effective options are becoming available, giving hope to those living with this challenging condition.